By Andreas Moritz
Coronary heart disease and heart attacks take more American lives than any other cause. Although it occurs suddenly, a heart attack is actually the final stage of an insidious disorder that has been years in the making. The disorder is known as coronary heart disease. Since the disease plunders only prosperous nations and has rarely killed someone before 1900, we have to hold our modern lifestyles, unnatural foods and unbalanced eating habits responsible for today’s heartsick society. But long before the heart begins to malfunction, the liver loses much of its major vitality and efficiency.
The liver influences the entire circulatory system, including the heart. In fact, it is the greatest protector of the heart. Under normal conditions, the liver thoroughly detoxifies and purifies venous blood that arrives via the portal vein from the abdominal part of the digestive system, the spleen and the pancreas. Apart from breaking down alcohol, the liver detoxifies noxious substances, such as toxins produced by microbes. It also kills bacteria and parasites, and neutralizes certain drug compounds with the help of specific enzymes. One of the liver’s most ingenious feats is to remove the nitrogenous portion of amino acids, since it is not required for the formation of new protein. It forms urea from this waste product. The urea ends up in the blood stream and is excreted in urine. The liver also breaks down the nucleoprotein (nucleus) of worn-out cells of the body. The byproduct of this process is uric acid, which is excreted with urine as well.
The liver filters more than a quart of blood per minute, leaving only the acid carbon dioxide for elimination through the lungs. After it is purified in the liver, the blood passes through the hepatic vein into the inferior vena cava which takes it straight into the right side of the heart (see Figure 1). From there the venous blood is carried to the lungs, where the interchange of gases takes place: carbon dioxide is excreted and oxygen absorbed. After leaving the lungs, the oxygenated blood passes into the left side of the heart. From there it is pumped into the aorta. The aorta supplies all body tissues with oxygenated blood.
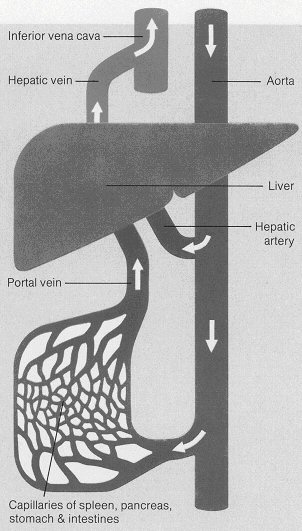 Figure 1: The way the liver filters blood
Figure 1: The way the liver filters blood Gallstones in the bile ducts of the liver distort the basic framework of the lobules. Consequently, the blood vessels supplying these liver units develop kinks, which greatly reduces internal blood supply. Liver cells become damaged, and harmful cellular debris begins to enter the blood stream. This further weakens the liver’s ability to detoxify the blood. As a result, more and more harmful substances are retained both in the liver and in the blood. A congested liver can obstruct the venous blood flow to the heart, leading to heart palpitations or even heart attacks. It is obvious that toxins which are not neutralized by the liver, end up damaging the heart and blood vessel network.
Another consequence of this development is that proteins from dead cells (about 30 billion per day) and unused food proteins are not sufficiently broken down, which, in turn, raises the protein concentration in the blood. Consequently, the body tries to store these proteins in the basement membranes of the blood vessel walls (further explanations of this scenario are given below). Once the body’s storage capacity for protein is exhausted, the extra proteins are forced to remain in the blood stream. This can cause the number of red blood cells to increase, which raises the packed cell volume of the blood, called hemocrit, to abnormal levels. The concentration of hemoglobin in the red blood cells also begins to increase, giving rise to a red complexion of the skin, particularly in the face and chest. (Hemoglobin is a complex protein that combines with oxygen in the lungs and transports it to all body cells.) As a result, the red blood cells become enlarged and are, therefore, too big to pass through the tiny channels of the capillary network. Obviously, this causes the blood to become too thick and slow moving, thereby increasing its tendency toward clotting (platelets sticking together).
The formation of blood clots is considered to be the main risk factor for heart attack or stroke. Since fat has no clotting ability, this risk stems mainly from the high concentration of protein in the blood. Researchers discovered that the sulphur-containing amino acid homocysteine (HC) promotes the tiny clots that initiate arterial damage and the catastrophic ones that precipitate most heart attacks and strokes (Ann Clin & Lab Sci, 1991 and Lancet 1981). Please note that HC is up to 40 times more predictive than cholesterol in assessing cardiovascular disease risk. HC results from normal metabolism of the amino acid methionine, which is abundant in red meat, milk and other dairy products. High concentrations of protein in the blood hinder the necessary constant distribution of important nutrients, especially water, glucose and oxygen to the cells.
The proteins also undermine complete elimination of basic metabolic waste products (see section ‘Poor Circulation, . .’). All of these factors combined force the body to raise its blood pressure. This condition, which is commonly known as hypertension, reduces the life-endangering effect of blood thickening, to some extent. However, this life-saving response to an unnatural situation unduly stresses and damages the blood vessels.
One of the body’s first and most efficient tactics for avoiding the danger of an imminent heart attack is to take excessive proteins out of the blood stream and store them elsewhere, for the time being (see Figure 2). The only place where protein can be accommodated in large quantities is the blood vessel network. The capillary walls are able to absorb most of the extra protein. They rebuild the protein into collagen fiber, which is 100% protein, and store it in their basement membrane. The basement membrane has the capacity to increase its thickness by 10 times before its storage capacity for protein has been exhausted. But this also means that the cells in the body no longer receive adequate amounts of oxygen and other basic nutrients. The cells affected by the ‘starvation in progress’ may also include cells that make up the heart muscles. The result is heart muscle weakness and reduced performance of the heart and, of course, any kind of degenerative illness, including cancer.
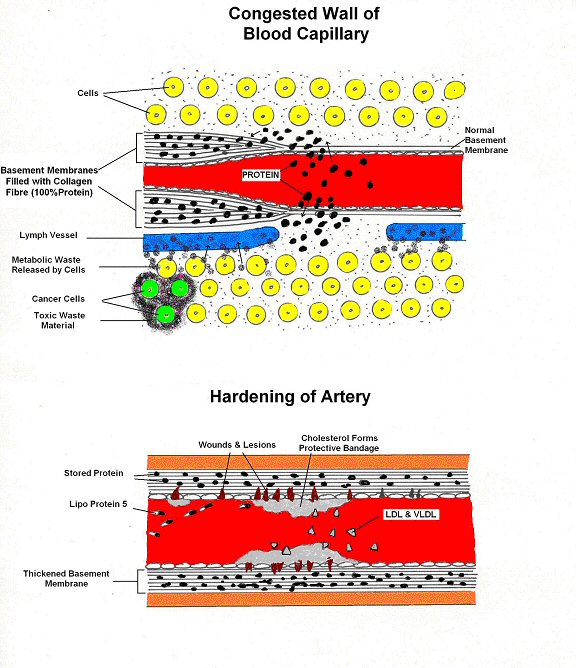 Figure 2: The beginning stages of heart disease
Figure 2: The beginning stages of heart disease When no more protein can be accommodated in the capillary walls, the basement membranes of the arteries also start absorbing protein. The beneficial effect of this action is that the blood remains thin enough to avert the threat of a heart attack, at least for some time. But eventually, the very same tactic that prevents death damages the blood vessel walls (only the primary survival mechanisms of the body are without major side-effects). The inner lining of the artery walls becomes rough and thick, like rust in a water pipe. Cracks, wounds and lesions show up at different locations.
Smaller blood vessel injuries are dealt with by blood platelets. They release the hormone serotonin, which helps to constrict the blood vessels and reduce bleeding. But larger wounds, as they are typically found in diseased coronary arteries, cannot be sealed by platelets alone; they require the body’s complex process of blood clotting. However, if a blood clot breaks loose, it can enter the heart and result in myocardial infarction, commonly called a heart attack. [Note: A clot that reaches the brain results in a stroke. One that blocks the opening into the pulmonary arteries, which deliver used blood to the lungs, can be fatal.]
To prevent the danger before it arises, the body uses an entire arsenal of first aid measures, including the release of the blood chemical lipoprotein 5 (LP5). Due to it sticky nature, LP5 works as a ‘band aid’ and creates a firmer seal around the wounds. As a secondary but equally important rescue operation, the body attaches specific types of cholesterol to the damaged sites (more on this in the section ‘High Cholesterol’). This acts as a more reliable patch-up or bandage. But since cholesterol deposits alone aren’t protection enough, connective tissue and smooth muscle cells also begin to build up inside the blood vessel. Called athersclerotic plaques, these deposits can eventually occlude an artery completely, obstructing the flow of blood and promoting the formation of deadly blood clots. When the blood supply to the heart is cut off, heart muscle activity stops and a heart attack is the inevitable result. Although the gradual destruction of blood vessels, known as atherosclerosis, initially protects a person’s life against a blood clot-caused heart attack, it is eventually also responsible for causing one.
——————————
You may share or republish this article provided you clearly mention the name of Andreas Moritz and paste a hyper link back to the web page